Alzheimer’s-in-a-Dish: New Tool for Drug Discovery
Posted on by Dr. Francis Collins
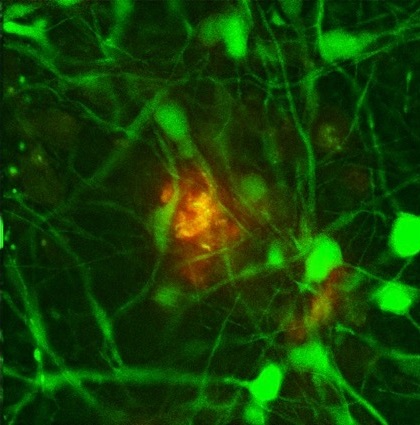
Credit: Doo Yeon Kim and Rudolph E. Tanzi, Massachusetts General Hospital/ Harvard Medical School
Researchers want desperately to develop treatments to help the more than 5 million Americans with Alzheimer’s disease and the millions more at risk. But that’s proven to be extremely challenging for a variety of reasons, including the fact that it’s been extraordinarily difficult to mimic the brain’s complexity in standard laboratory models. So, that’s why I was particularly excited by the recent news that an NIH-supported team, led by Rudolph Tanzi at Boston’s Massachusetts General Hospital, has developed a new model called “Alzheimer’s in a dish.”
So, how did Tanzi’s group succeed where others have run up against a brick wall? The answer appears to lie in their decision to add a third dimension to their disease model. Previous attempts at growing human brain cells in the lab and inducing them to form the plaques and tangles characteristic of Alzheimer’s disease were performed in a two-dimensional Petri dish system. And, in this flat, 2-D environment, plaques and tangles simply didn’t appear.
After a series of futile attempts using a 2-D system, Doo Yeon Kim, a researcher in Tanzi’s lab, suggested the team try to grow human neural stem cells in a 3-D gel matrix. And, voila, that did the trick! The gel system allowed the cells to grow more naturally and form into 3-D networks just like they do in the brain—which, as we all know, just happens to be 3-D.
Admittedly, it took a bit more than the magic of a 3-D gel to create this innovative model. The Boston team used genetic engineering to spur the neural stem cells to produce two specific proteins that are the hallmarks of Alzheimer’s disease: β-amyloid and tau. In the brains of people with Alzheimer’s, excessive accumulation of β-amyloid results in the formation of plaques in the spaces between neural cells, while tau is the main component of destructive neurofibrillary tangles within the cells. Until the latest achievement, no single model of Alzheimer’s disease simultaneously contained both amyloid plaques and neurofibrillary tangles.
To demonstrate the utility of their new Alzheimer’s-in-a-dish model, the Tanzi team showed that blocking the formation of amyloid plaques with certain drugs prevents tau tangles from forming inside the neurons. This lends support to the 30-year old hypothesis that plaques are the early culprits in Alzheimer’s disease, triggering a cascade of events leading to the tangles. This finding also provides new encouragement that this category of drugs (called beta-secretases and gamma-secretases) might ultimately provide benefit to patients if given early enough in the course of the disease.
In addition to the many ways in which this new model can be used to expand our understanding of Alzheimer’s disease, I’m excited about its applications for drug discovery and development. Plaques and tangles appear in this 3-D model in just six weeks, quite a contrast to the one year that it takes for plaque alone to form in a mouse model. This should greatly accelerate our efforts to screen for potential therapies that may slow, halt, or possibly even prevent the destructive march of Alzheimer’s disease throughout the brain.
In fact, Tanzi plans to use his new model to test 1,200 drugs that are already approved by the Food and Drug Administration for other diseases, with the goal of seeing whether any of these drugs might be put to a new use against Alzheimer’s. He also plans to test 5,000 experimental drugs for additional leads.
Hopefully, “Alzheimer’s in a dish” is just the first in a long series of success stories for modeling a wide variety of brain diseases. In their paper in the journal Nature, the researchers say that their unique strategy should serve to facilitate the development of better models for other neurodegenerative disorders.
Reference:
[1] A three-dimensional human neural cell culture model of Alzheimer’s disease. Choi SH, Kim YH, Hebisch M, Sliwinski C, Lee S, D’Avanzo C, Chen H, Hooli B, Asselin C, Muffat J, Klee JB, Zhang C, Wainger BJ, Peitz M, Kovacs DM, Woolf CJ, Wagner SL, Tanzi RE, Kim DY. Nature. 2014 Nov 13;515(7526):274-8.
Links:
Alzheimer’s Disease Fact Sheet (NIA)
Alzheimer’s Disease: Unraveling the Mystery (NIA)
Tanzi Lab, Massachusetts General Hospital, Boston
NIH support: National Institute on Aging (NIA), National Institute of Mental Health, National Institute of Neurological Diseases and Stroke

We have to work hard to find small molecules that can interact with proteins, which are large molecules. Small molecule drugs are preferred by pharmaceutical companies because they are relatively easy to make, and can often be taken orally